Researchers at Amsterdam UMC have developed an algorithm that supports general practitioners in the early detection of lung cancer. Thanks to the use of artificial intelligence (AI), it is possible to identify patients with an increased risk up to four months earlier than with current methods. In doing so, they are taking an important step toward data-driven, personalized primary care.
The British AI model differs from other models that typically only look at coded variables such as “smoking” or “hemoptysis” (coughing up blood). In addition to structured data, the newly developed AI model can also analyze free text in electronic patient records. Thus, the algorithm is able to recognize patterns in open text fields. These often contain valuable but unstructured information that was previously not automatically exploited. “In the medical history, the algorithm detects subtle signals that indicate an increased risk of lung cancer,” explains Prof. Dr. Martijn Schut, professor of Translational Artificial Intelligence at Amsterdam UMC.
Smart algorithms in primary care
Deploying smart algorithms in GP consultations will create scope for faster diagnosis, timely treatment and potentially better outcomes for thousands of patients with lung cancer - and, in the future, perhaps other cancers as well.
According to Prof. Ameen Abu Hanna, professor of Clinical Informatics and co-investigator, this is an important step forward: “We show that hidden in free text is data that, with the help of AI, contributes to much earlier detection of cancer.” The study's findings were recently published in the British Journal of General Practice.
The importance of early diagnosis
The clinical impact of the algorithm is potentially significant. Of patients with lung cancer, nearly two-thirds (62%) were referred up to four months earlier than in routine care practice. A relevant time gain, since most diagnoses now occur at stage 3 or 4 of the disease - stages where prognosis is often poor and treatment options are limited and four in five (80%) of patients usually die within one year of diagnosis. “An earlier start of treatment - even of just four weeks - can have a noticeable effect on survival. A gain of four months is therefore particularly promising,” said Henk van Weert, Emeritus Professor of Family Medicine.
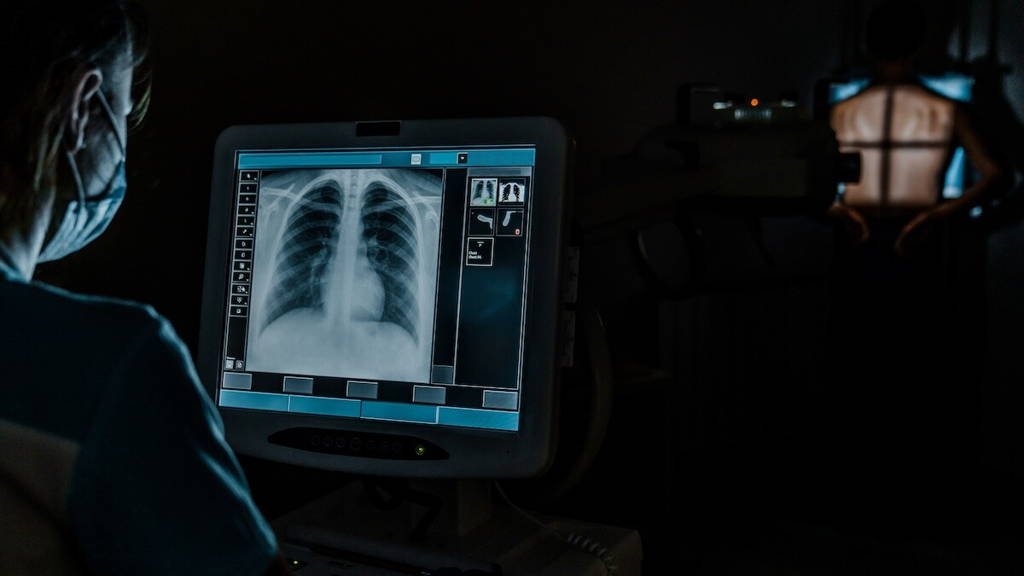
Much research is being done worldwide on the added value and gains AI technology can bring to medical diagnostics. For example, British researchers, in collaboration with the Dutch Research Institute for Diagnostic Accuracy, recently examined the effectiveness of a Korean AI tool for analyzing lung scans for lung cancer. This tool successfully identified scans without significant lung nodules, allowing radiologists to focus their attention on cases that required further analysis. A key finding was that all confirmed cases of lung cancer were part of the scans flagged by the AI for further investigation, suggesting that no diagnoses were missed.
Effective and practical
The British AI algorithm was tested on data from more than 525,000 patients from four academic GP networks in Amsterdam, Utrecht and Groningen. Of this group, 2,386 patients were diagnosed with lung cancer, validated through the Dutch Cancer Registry.
Remarkably, the algorithm is not only effective, but also practical. The risk assessment can take place during the regular consultation, without additional burden on either GP or patient. Of every 34 patients identified, an average of one was found to actually have lung cancer. This is a significantly more favorable ratio than with regular population screening.
Follow-up research
Although the current model was developed specifically for lung cancer, the researchers see potential for applying this approach to other hard-to-detect cancers such as pancreatic, stomach and ovarian cancer. There, early detection is often even more challenging, with major implications for prognosis. Follow-up research is needed for actual implementation. Validation in other healthcare systems and countries is essential to ensure the robustness and generalizability of the model.
Last year, researchers at Leiden University Medical Center (LUMC) developed an AI model that can more accurately and cost-effectively predict the risk of uterine cancer recurrence, compared to existing methods for doing so. Those outcomes can be used to improve, and personalize, treatment plans. LUMC's AI model, HECTOR, analyzed microscopic images of tumors and data from previous clinical trials. Although additional research is needed, researchers already saw HECTOR last year as an important step in the technological revolution within oncology, with potential for improved patient care and survival rates.