For the first time in history, researchers at Leiden University Medical Centre (LUMC) and their French colleagues have succeeded in using a newly developed technique to see and measure the smallest blood vessels in the brain. This new technique can help with the early detection and treatment of neurological diseases such as Alzheimer's, Parkinson's, diabetic vascular dementia and hereditary diseases such as HHT, CADASIL and RVCL-S. This makes it possible to intervene before irreversible brain damage occurs.
This opens up avenues for new treatments that can be used before the disease fully develops. The findings have been published in the scientific journal Nature Biomedical Engineering. The researchers have developed a device that allows them to view the smallest capillaries in the brain (brain capillaries) in high resolution. This allows them to see not only their shape, but also their function. They can see how the blood flows, how the vessels respond and whether there are any abnormalities.
Extremely small vessels
With current medical imaging techniques, such as MRI, CT scans or standard ultrasound, only the larger blood vessels are visible. Yet 80 percent of our circulatory system consists of capillaries. These are extremely small vessels with a diameter of up to 5 micrometres (0.005 millimetres). Until now, these capillaries were invisible. ‘There was no device to look at the smallest blood vessels deep inside organs. The best equipment we had could zoom in to 0.1 millimetres,’ says lead researcher Franck Lebrin.
Blood vessels transport blood throughout the body. They carry oxygen-rich blood from the heart to organs and tissues and return oxygen-depleted blood to the heart and lungs. The smallest blood vessels, the capillaries, are crucial in this process: they deliver oxygen and nutrients directly to the cells. This enables cells to function properly and remain healthy.
Oxygen deficiency
Sometimes these capillaries do not function as they should. In the brain, this can have serious consequences. Poor capillary function can lead to oxygen deficiency, the intrusion of harmful substances and persistent inflammation. This process can cause irreversible brain damage, which can ultimately lead to dementia. The problem is that the symptoms usually only become apparent when the damage is already too advanced to be treated. However, the first changes in capillaries often begin up to twenty years before the first symptoms of brain damage become apparent. With the newly developed device, researchers can now visualise these early abnormalities.
This technique is based on an advanced form of ultrasound. According to researcher Lebrin, the device is much more precise than previous methods. ‘Imagine the blood vessels of the brain as a road network. Previously, we could only see the motorways. Now, the provincial roads, streets and even country lanes are also visible. We have gone from 20 per cent to 95 per cent visibility in one fell swoop,’ Lebrin says enthusiastically. She expects that it will soon be possible to make the last 5 per cent of the capillaries visible as well.
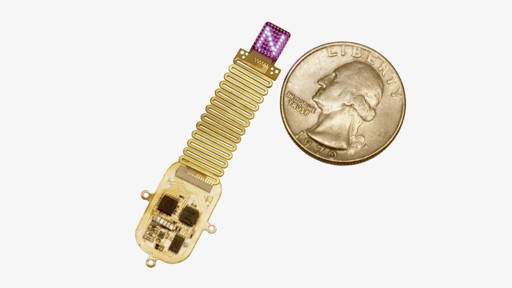
Helmet
The new technique works via a type of helmet that is placed on the head and scans the brain. No surgery is required, making the examination completely non-invasive. In the laboratory, the method has been successfully tested on mice with HHT: a rare hereditary condition in which the capillaries are fragile and dilated and bleed easily. The cause often lies with so-called pericytes. These are cells that normally stabilise the small blood vessels and ensure the proper functioning of the blood-brain barrier. When these cells fail, problems arise.
The device enabled researchers to produce razor-sharp images of changes in the blood vessels, blood flow and the formation of abnormal connections. Because the smallest capillaries in mice and humans are the same size, the results are expected to be easily transferable to humans.
Application in patients
Later this year, a study will start in patients with RVCL-S, a rare hereditary disorder that affects the small blood vessels. This will be done in collaboration with the Neurology Department of the LUMC. At the same time, Lebrin's research group will start testing new experimental drugs that target pericytes. Thanks to the new device, they will be able to measure the effect of these drugs directly on the brain vessels. The test subjects carry the genetic mutation for RVCL-S or HHT, but do not yet have any symptoms. This allows researchers to intervene before the disease actually manifests itself.
Although the research starts with HHT, the potential of the technique is much greater. According to Lebrin, the device could also be used in the future to examine blood vessels in other organs, such as the heart and kidneys. At the LUMC, the technology is already being used in organ donation to check whether a donor kidney has good blood flow. In the future, the method could also help to detect other diseases involving vascular problems at an early stage.
From lab to practice
The research is a collaboration between the LUMC and the Institute of Physics of Medicine in Paris (part of the French institute Inserm), which developed the clinical system. This collaboration led to the establishment of an International JointLab and a spin-off company that focuses on treatments that target pericytes. The project, called MICROVASC, is funded by the European Innovation Council (EIC) within the European Union's EIC Pathfinder Challenge.