Dr. Theresa McDonnell, SVP & Chief Nurse Executive at Duke University Health System, explains how innovation, AI-driven tools, and frontline collaboration are reshaping the nursing workforce. She describes a future where nurses are not just adapting to change – they are leading it.
Dr. McDonnell, Duke University Health System has become a leader in addressing nursing workforce challenges through innovation. Can you walk us through your staffing model and how it’s helping reduce burnout and improve retention?
We approach workforce design as an opportunity to activate nursing insight and innovation. Our AI-driven scheduling model dynamically aligns staffing to patient demand, improving retention by 18% and reducing overtime by 23%. However, the real innovation comes from how we co-develop these tools with nurses themselves.
Duke nurses aren’t just using technology but designing it. Through platforms like our Nurse Innovation Summit, staff have created impactful solutions like VR-based safety training and smart IV pump standardization. These innovations improve care because they’re built by those closest to it.
We’ve also strengthened academic-clinical integration, relocating Watts College of Nursing to our campus to foster systems thinking from day one. This model positions nurses as critical architects of healthcare’s future, not just in response to change, but as the ones driving it.
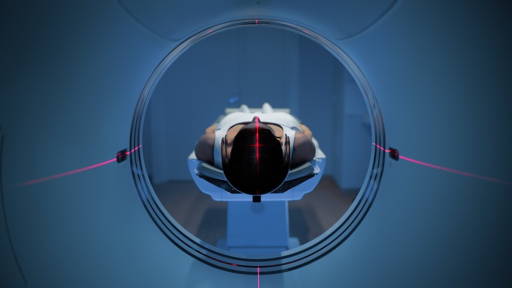
AI-powered patient monitoring is a relatively new frontier in healthcare. How are Duke nurses responding to these tools? Are they embracing AI as a partner in care? What steps have you taken to ensure technology enhances rather than overwhelms their daily work?
Our staff are shaping how we implement AI-powered tools. AI is an opportunity to strengthen, not substitute, clinical expertise. Our patient monitoring systems leverage predictive analytics to surface early warning signs and support safer care decisions, but these systems are co-designed with clinical teams to ensure relevance.
We are implementing ambient listening and documentation tools that have the potential of cutting admin time by up to 40%, allowing nurses to focus on patient interaction. The key is alignment: technology must reflect the realities of clinical workflows.
By engaging nurses from the start, we’ve built a culture where innovation feels empowering, not imposed. This partnership ensures AI enhances care delivery while reinforcing nurses’ role as critical decision-makers in modern healthcare.
You’ve championed frontline-led innovation through nursing hackathons. Can you share a few standout examples where this approach led to meaningful improvements in patient care or workflow efficiency?
Our Nursing Innovation Summits have produced robust, nurse-designed solutions with measurable impact. One standout is a virtual reality training platform for de-escalating workplace violence, which has delivered over 5,000 hours of training and reduced incidents system-wide.
Another is the Smart IV Pump Standardization initiative, which lowered medication errors by 19% by streamlining workflows and reducing variability. Our bedside interpretation tool, developed by nurses, improves communication during critical moments, especially for non-English-speaking patients.
By giving nurses the tools and support to prototype and implement their ideas, we’ve created a culture where innovation is part of everyday practice.
Many healthcare workers are understandably cautious when it comes to adopting new technologies. What’s your approach to building trust and enthusiasm for innovations like AI-driven tools among your nursing teams?
Trust starts with inclusion. We invite nurses to create innovations rather than ask them to adopt them. From the earliest stages, our teams are involved in designing, testing, and refining tools like AI-supported scheduling and ambient documentation. That shared ownership builds confidence and clarity.
We also invest in education that demystifies AI, positioning it as a clinical partner among nurses. We have seen that when nurses see that technology can eliminate friction points and amplify its impact, enthusiasm follows naturally.
Adopting new technologies isn’t about convincing nurses to embrace change but empowering them to lead it. When innovation reflects the real-world needs of the people who use it, adoption becomes a byproduct of trust and relevance.
From your experience, how can health systems balance the push for digital transformation with the human, relational side of nursing, which is so central to patient care?
Digital transformation and human connection are interdependent. We view technology as a means to elevate the relational core of nursing. Tools like ambient documentation and AI-assisted discharge planning reduce administrative load, allowing nurses to reposition their time to build trust, listen deeply, and educate patients and families.
We balance innovation by grounding every decision in clinical relevance. Staff help define how tech is deployed, ensuring it supports, not disrupts, the patient experience.
The future of care isn’t less human; it’s more focused. When digital tools are thoughtfully integrated, they free nurses to do what only nurses can: deliver relational, intuitive, person-centered care at the highest level.
What role do you believe nurses should play in shaping and co-developing new healthcare technologies, and how does Duke empower them to be part of that conversation?
Nurses should be at the table from day one, co-developing technology, not retrofitting it. They bring unmatched proximity to patient needs and system gaps, making their insight essential to building tools that actually work in practice.
We are building structures that reflect this belief. Through hackathons and innovation summits, nurses collaborate with engineers, developers, and operational leaders to design solutions grounded in frontline experience. Their ideas have led to innovative tools and more intuitive workflows.
We see our nurses as architects for the future of healthcare. When innovation is driven by those closest to care, it leads to better outcomes, stronger teams, and lasting transformation.
Technology evolves fast, but clinical adoption can be slow. What lessons has Duke learned about scaling new tech solutions, like AI monitoring or predictive staffing, across a large health system without creating disruption or resistance?
Scaling tech in healthcare is about strategy. We’ve learned that successful adoption starts with alignment: solutions must solve real clinical problems and reflect the input of those delivering care.
We pilot in focused environments with high feedback loops, engaging nurses early to refine usability before broader rollout. This builds credibility and avoids resistance from our teams.
We also embed innovation teams into clinical units so that implementation feels collaborative, not imposed. With predictive staffing, for example, our nurses helped shape workflows, identify friction points, and co-own the rollout.
By strategizing our technology rollouts in this sense, adoption doesn’t stall when nurses feel like partners in transformation.
As AI, robotics, and digital platforms continue to evolve, how do you personally envision the future of nursing over the next decade? Will the role look fundamentally different, or will technology be another layer of support for the human heart of care?
The role of nursing will absolutely evolve, but not away from its core. Over the next decade, I see nurses taking on even more strategic, systems-level influence. I see nurses leading AI integration, co-designing care delivery models, and driving global health innovation.
I hope technology will become second nature, ambient, adaptive, and seamlessly embedded into practice. I don’t foresee it replacing what makes nursing powerful. If anything, it will amplify it.
The future nurse will be clinically expert, tech-savvy, and innovation-minded. But most importantly, they’ll be at the center of shaping what care looks like. We’re not moving past the human heart of nursing. We’re building from it with greater clarity, capability, and collective impact.